If you are receiving home health care (also called home health services), this means that you need some medical care, but not enough to be admitted to a hospital or skilled nursing facility.
There are several advantages to receiving home care, such as you:
- Aren’t exposed to the microbes (germs) that may circulate in the facility.
- Have less frequent person-to-person contact with staff, volunteers, and others patients who could expose you to an infection.
- Are in a familiar and more comfortable environment.
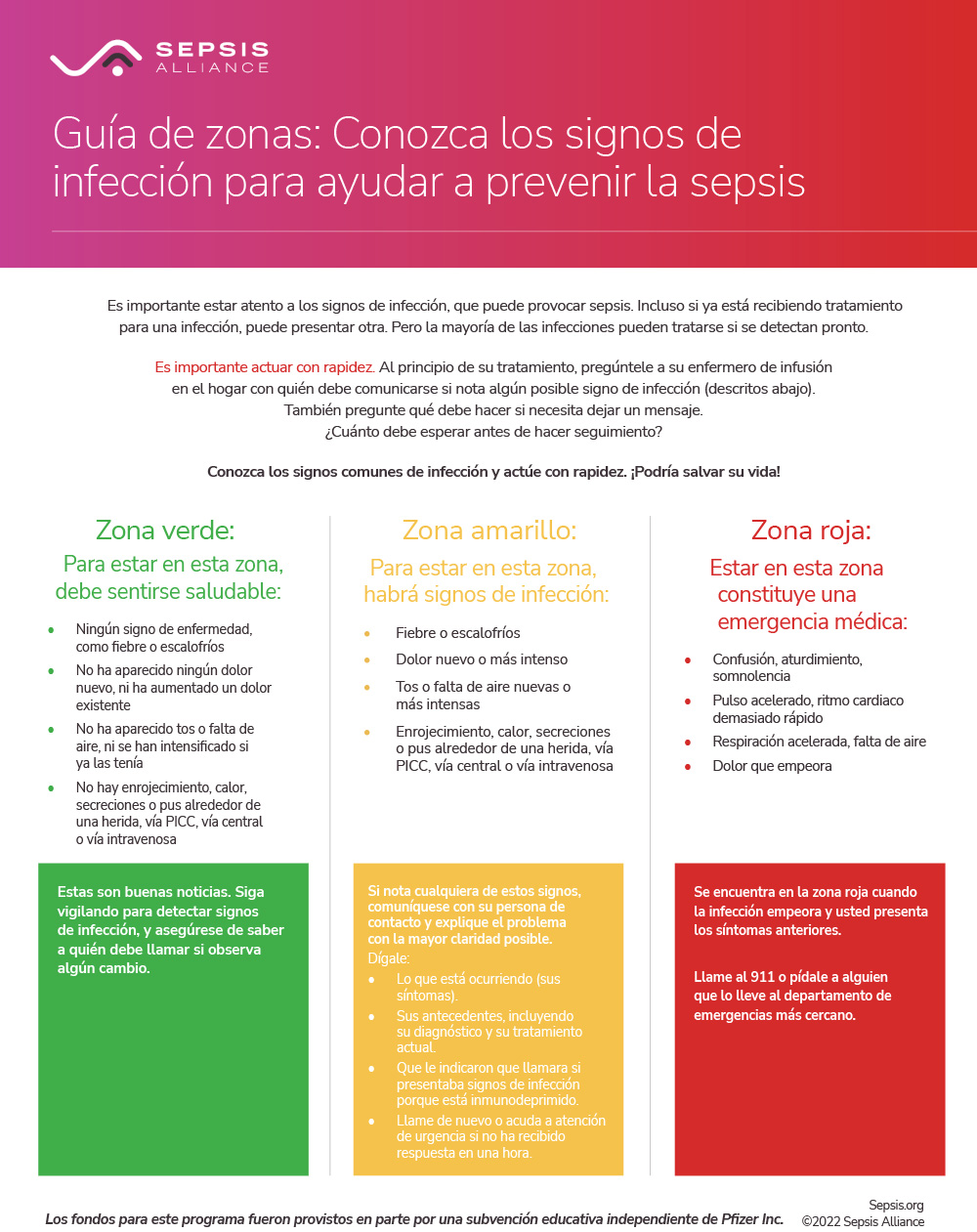
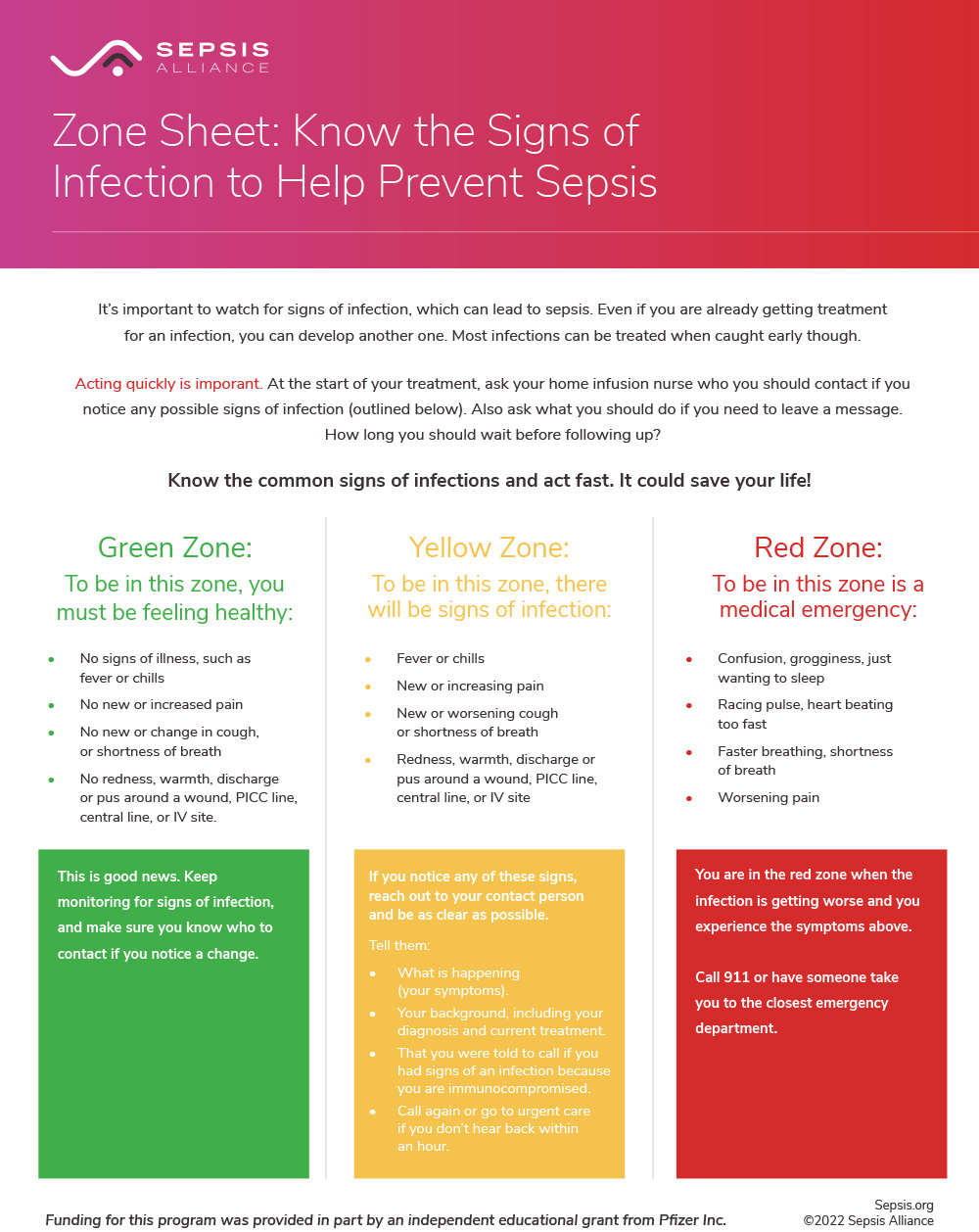
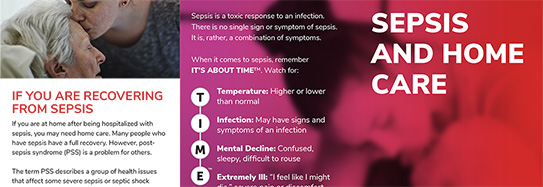
However, there is still a risk that you could contract an infection while you are receiving home care. Any type of infection could cause sepsis. If you are a caregiver to someone receiving home care, this information is important for you as well. Sepsis, which was often called blood poisoning, is the body’s life-threatening response to infection. Like strokes or heart attacks, sepsis is a medical emergency that requires rapid diagnosis and treatment.
Suggested Citation:
Sepsis Alliance. Sepsis and Home Care. 2023. https://staging.sepsis.org/sepsisand/home-care/
Updated October 25, 2023.